Clinical Examples: Percutaneous Pin Stabilization with Thermoplastic Bonding
|
Percutaneous skeletal stabilization is commonly used in
hand surgery, and has the advantage of minimal soft
tissue disruption. Pins may be left protruding through
the skin or cut short enough that the ends lie beneath
the skin. There are pros and cons of each technique
relating to infection risk and details of pin removal. One issue is that smooth pins are used, and may loosen or migrate. One solution to this is to leave the pins protruding through the skin, bend them to create a zone of overlap and glue the overlap together with thermoplastic splint material. This prevents pin migration and improves long term stability of the fixation. These cases demonstrate this technique in different scenarios of percutaneous fracture pinning. There are many other different options for each of these injury patterns. |
| Click on each image for a larger picture |
|
Case 1
Distal phalanx grossly mobile nonunion 8 weeks following fingertip
crush injury. |


| New nail plate
growing deep to the existing nail. |

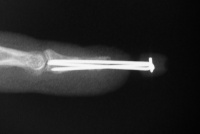
| The fracture was
reduced and stabilized with three pins left protruding
through the fingertip. |

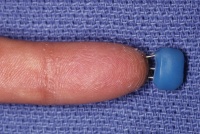
| Four weeks postop,
immediately prior to pin removal. A small space is left
between the skin and thermoplastic join to allow for
swelling and cleaning. |


| Late result. |






|
Case 2
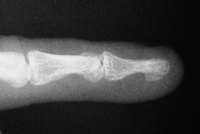
Distal phalanx delayed union with appearance of
probable soft tissue interposition. |

| Unable to achieve
closed reduction. |

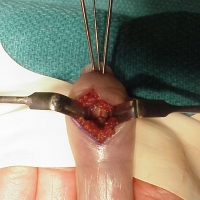
| Fracture exposed
through a palmar approach and soft tissue
interposition removed. |



| Reduction and
stabilization. |




|
Case 3
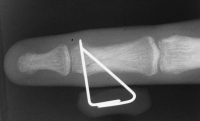
Acute mallet fracture treated with percutaneous
pinning: proximal pin stabilizes the fracture
fragment, longitudinal pin maintains distal phalanx
position. |

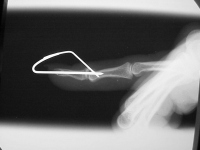
| Thermoplastic bonding of the protruding ends: appearance at one month. |



| Late result. |
|
Case 4
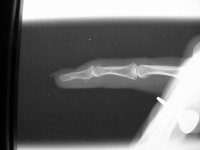
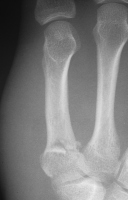
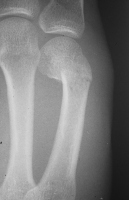
Rotated unstable spiral oblique proximal phalanx
fracture. |


| Reduction and fixation. |
| Appearance at four
weeks. |




| Late result. |



|
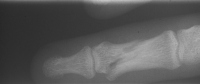
Case 5
Young man sustained bilateral metacarpal fractures.
The left hand injury included a small metacarpal base
comminuted fracture subluxation. |


| Percutaneous
fixation. |
| Thermoplastic
stabilization. |

| The right hand sustained a small metacarpal neck fracture with palmar angulation. |
| Reduction and
fixation. |

| Pin
stabilization. |

| Pins were
removed at four weeks. Appearance at eight weeks
after surgery. |


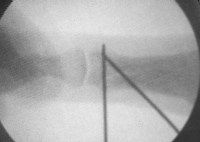
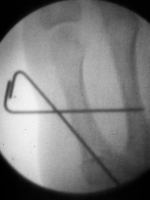
| Case 6 Extraarticular distal radius fracture with angulation and dorsal comminution. |


| Attempts at
closed reduction alone were unsuccessful. |

| Freer elevator
introduced percutaneously as a reduction aid. |


| Percutaneous
fracture stabilization with three pins via the
dorsal radial tubercle, radial styloid and FCR
portals. |


| Pins were left
protruding and bent to overlap. |

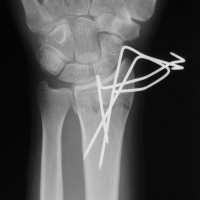
| Thermoplastic-pin
construct at 6 weeks, immediately prior to removal. |



| Late result. |





|
Search for... |
Case Examples Index Page | e-Hand home |