Harvesting a
full thickness or thick split thickness graft free hand
with primary closure of the donor defect is not difficult. This is one
way of doing this, harvesting skin from the inguinal crease. The same
approach can be used for forearm or lower abdomen donor sites:
- Make a template of the wound from a piece of Esmarch or
glove paper cut to
fit the defect.
- Mark the superficial side of the template with a marker so
that you don't use it upside down
- Center the longest axis of the template along the inguinal
crease.
- Position the template so that you won't be using skin with
pubic hair, usually lateral to the femoral pulse.
- Find the widest area area which will need to be closed and
pull the skin from these future edges with skin hooks across the
anticipated defect to make sure that they can touch in the areas of the
anticipated closure to confirm that you will be able to bring these
future edges together.
- Draw an outline around the template in a lenticular
(ellipse with pointed ends) shape. The length:width ratio of the
lenticular shape must be at least 3:1 to avoid dog ears. This will
include areas of skin to be discarded, which can include hair bearing
skin in the corner.
- Infiltrate the donor entire area with 1% lidocaine with
1:100,000
epi.
- Go back to the wound, tidy up, get "perfect" hemostasis.
This will give time for the epi to kick in. More importantly, the
condition of the wound bed - bacterial count, poor vascularity, gross
motion - is the entire determinant of whether the graft will adhere or
not. If the bed is bad, it doesn't matter what type of bolster or
bandage you put on.
- Harvest the graft. This requires a good assistant,
hemostats and a steady supply of new scalpel blades.
- Superficially incise the outline of the skin to be excised,
not all the way through the dermis.
- 3 hemostats: One (you hold) on the tip of the graft; the
other two an inch back on the edges of the graft for your assistant.
Pull these to tension the triangular area defined by their attachments
and lift up.
- Use your scalpel to develop a plane through the deep
dermis, leaving a thin deep layer of dermis. The right level will have
little yellow fat pinpoints on the donor site dermis, but none on the
graft. Very similar to elevating a thin skin flap during fasciectomy
for Dupuytren's in an area where there is dense dermal involvement.
See? you've done this before!
- As you progress, you and your assistant use the
hemostats to pull the graft up, not back - don't fold the graft
backward or you will buttonhole it at the fold.
- As you progress, keep repositioning the two assistant
hemostats to keep the area where you are working tight like a drum head.
- Swap out scalpel blades frequently - makes it faster and
easier.
- Once done, trim off any fat from the undersurface of the
graft with scissors.
- Intradermal closure will be appreciated by the patient and
your office staff. I use interrupted deep 3-0 vicryl to line things up,
then running 5-0 monocryl, steri strips, adaptic, tegaderm, opsite for
final closure.
- Trim the graft to the defect and close.This is the only
time I use horizontal mattress sutures - they maximize the contact of
the graft dermis to the bed. No bubbles, no bleeding allowed at the end.
- A sew on bolster is unnecessary unless the defect is quite
concave - I normally use adaptic, saline moistened gauze, dry gauze and
gauze wrap. and a splint. The science is that capillary ingrowth
requires less than 6 microns of shear motion at the interface for the
graft to survive. Fibrin in the wound, not an exterior bolster, is the
only thing that can accomplish this. Absent gross motion, the graft
will either stick or not stick depending on the condition of the
recipient bed.
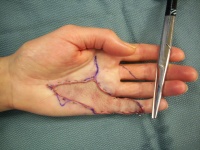
I use this routinely for skin grafts of the hand. Three donor sites are
available: longitudinal medial forearm (small); inguinal crease
(medium); transverse lower abdomen (larger)
The other option is to go for a full thickness graft by harvesting a
full thickness piece of skin and fat, close the donor defect any way
you like, then meticulously cut the fat from the deep dermis with the
convex side of sharp curved scissors. Less learning curve, but it beats
up the graft undersurface more than the above approach.
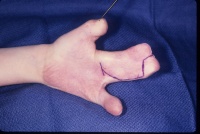
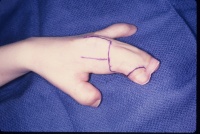
The following cases illustrate some of the details of this technique.
|